ARCHIVES of Medical and Biomedical Research

p-ISSN 1694-2086
| Arch Med Biomed Res. 2014;1:129-138. doi:10.4314/ambr.v1i4.2 | |
Sero-prevalence of IgM antibody to Rubella Virus in pregnant women in Zaria, Nigeria Okikiola Olajide1, Maryam Aminu1, Abdullahi J Randawa2, Daniel S Adejo2
correspondence to Received: July 04, 2014
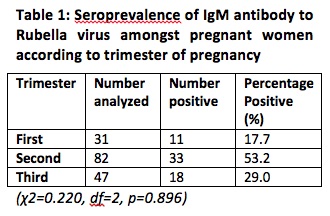
INTRODUCTION Rubella also known as German measles is a contagious viral infection that is caused by Rubella virus, a member of the family Togaviridae1. The virus causes a mild rash-like disease that is associated with low-grade fever, lymphadenopathy and a short-lived morbilliform rash2. Rubella is predominantly a childhood disease which is endemic throughout the world1,3-5. In contrast to the mild infections caused in early childhood or adult life, rubella in pregnant women causes Congenital Rubella Syndrome (CRS), which is the infection of a developing foetus following transplacental transmission of rubella virus from the mother to the foetus2. Complications can occur in an unborn baby if the mother becomes infected during pregnancy, resulting in a miscarriage, stillbirth or a child born with birth defects6. In the first 3 or 4 months of pregnancy, rubella infection provides opportunities during the period of maternal viremia for invasion of the placenta and subsequent fetal infection7. The risk to a fetus is highest in the first few weeks of pregnancy and then declines in terms of both frequency and severity, although some risks still exist in the second trimester8. After placental infection is established, there can be subsequent dissemination of virus to the fetus2. After entry, the virus is capable of spreading widely throughout the developing fetus, and almost any organ may be infected2,7. A chronic and generally non-lytic infection is then established in the fetus2. In the congenitally infected fetus and infant, virus persistence occurs in the presence of neutralizing antibodies; therefore immunological tolerance does not develop7. Although a comprehensive vaccination program in most industrialized regions such as North America, Europe, Japan and Australia has reduced the incidence of the disease in these areas to low levels, vaccination is not carried out in many developing countries2 including Nigeria. Epidemics occur every 6-10 years, with strong pandemics occurring every 20-25 years5. Epidemics in tropical countries usually pass unrecognized due to the lack of significant clinical symptoms in infected children2. One of the antibodies associated with rubella is the Immunoglobulin M (IgM) antibody. The IgM antibody rises and peaks 7-10 days after infection and then declines after several weeks. Therefore, the presence of IgM antibody indicates a recent infection, reinfection or false-positive IgM9,10. This study is aimed at detecting the presence of IgM antibody to Rubella virus in pregnant women in Zaria and also to compare seroprevalence between pregnant and non-pregnant women. Together with the clinical symptoms, risk factors and level of awareness assessed in the study, this study will provide information necessary for health care administrators and providers in Nigeria to initiate a nationwide rubella vaccination program. METHODOLOGY Study area and population A cross-sectional study was carried out between the months of June and August 2012, in the antenatal clinic of Ahmadu Bello University Teaching Hospital (ABUTH), Shika, Zaria, Nigeria. The hospital is a referral hospital that receives patients from all over Kaduna State and some neighboring states like Zamfara, Katsina and Kano State. 160 pregnant women in different trimesters of their pregnancy and 20 non-pregnant of childbearing age took part in the study. The non-pregnant women were involved in the study in order to compare prevalence between pregnant and non-pregnant women within the same community and to determine if exposure to infection occurs more frequently before or during pregnancy and also to establish if awareness of the infection was higher in an academic environment. Ethical approval for the study was obtained from the ethical committee of ABUTH and oral consent was obtained from both pregnant and non-pregnant women for their participation in the study. Blood samples were collected consecutively, once a week for a period of 7 weeks from the pregnant women and non-pregnant women were approached randomly within the university female hostels for a week. Prior to sample collection, structured questionnaires were administered to gather relevant medical information, obstetrical and socio-demographic characteristics from the women. Sample collection and processing A total of 180 blood samples were collected from 160 pregnant women and 20 non-pregnant women of childbearing age. Three milliliters of venous blood was collected from the women using standard aseptic technique into properly labeled plain bottles. The blood samples were allowed to stand at room temperature to allow for blood clotting after which samples were transported to the laboratory, centrifuged at 2500 revolutions per minute for 5 minutes and sera separated. The sera were stored at -20°C until analyzed. Analysis of samples All the serum samples were analyzed for anti-rubella IgM antibody using Sandwich Enzyme Linked Immunosorbent Assay (ELISA) commercial diagnostic kit (Diagnostic Automation, Inc. Immunodiagnostics, USA). The assay was carried out according to the manufacturer’s instructions. The results were read using a microplate ELISA reader (GF-M3000; B Bran Scientific & Instrument Co. England) and compared in a parallel manner with the calibrator and controls. Samples were interpreted as positive if their rubella IgM index was equal to or higher than the defined rubella IgM index, which was 1. All samples with an index of 0.90 or less were interpreted as negative and those with an index of 0.91-0.99 were equivocal. Analysis of results The data obtained from the questionnaires and the results of laboratory analysis were entered into Microsoft excel, analyzed using SPSS (statistical package for social sciences) version 16 and reduced to percentiles and figures. The Pearson Chi square test at 95% confidence interval and a significance level of 0.05 (p value ≤ 0.05) was used to determine the relationships between the demographic data and prevalence rates. RESULTS Seroprevalence of IgM antibody A total of 160 pregnant and 20 non-pregnant women took part in the study. Out of the 160 pregnant women, 62 (38.8%) were positive for rubella IgM antibody and 98 (61.2%) were negative. For the 20 non-pregnant women, 8 (40%) were positive for rubella IgM antibody and 12 (60%) were negative. 33 (53.2%) of the pregnant women who were positive were in their second trimester, 18 (29.0%) in their third trimester and 11 (17.7%) in their first trimester as shown in Table 1.
Age distribution and reproductive characteristics The age of the pregnant women ranged from 18 to 47 years (mean - 27.8 yrs) while that of the non-pregnant women was from 17 to 43 years (mean - 23.3 yrs) as shown in Table 2. More than half of the pregnant women (51.2%) were in their second trimester, with only 31 (19.4%) in their first trimester. Reproductive characteristics such as the number of term delivery, preterm delivery, life birth, still birth, spontaneous abortion, surviving children and malformed children were studied (Table 3). The mean of term delivery, pre-term delivery, life birth and surviving children are 2.8 (94/160, min. 1, max. 11), 1.1 (16/160, min. 1, max. 2), 2.7 (92/160, min. 1, max. 11) and 2.5 (89/160, min. 1, max. 8) respectively. 33 (20.6%), 14 (8.7%) and 4 (2.5%) of the pregnant women had history of spontaneous abortion, still birth and malformed children respectively. More than a quarter (28.1%) of the pregnant women had at least 5 children residing with them while even more (33.8%) had less than 5 children living with them. Most (103/160) of the pregnant women were educated up to the tertiary level and 78 of them were involved in occupation that involve children.
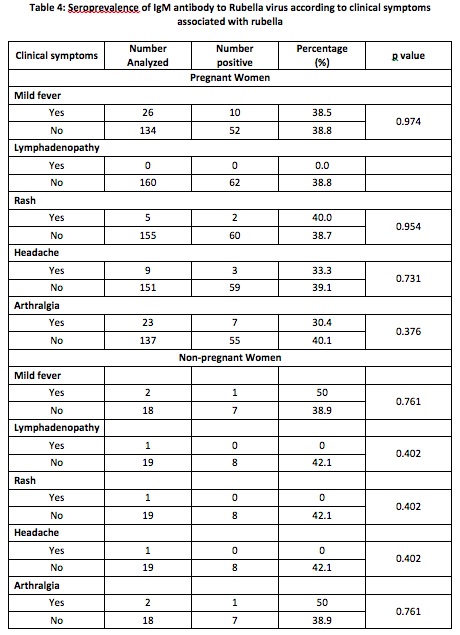
Clinical Symptoms and Awareness Both pregnant and non-pregnant women were observed for symptoms such as fever, swollen and tender lymph nodes, rash, headache and aching joints (Table 4). Of the 160 pregnant women 26 (16.2%), 23 (14.4%), 5 (3.1%) and 9 (5.6%) had fever, aching joints, rash and headache at the time of the study respectively. None of them had swollen lymph nodes at the back of their neck or behind their ears. Similarly, 1 (5%) of the non-pregnant women had rash, headache and swollen lymph nodes while 2 (10%) had fever and aching joints. Only 20 (12.5%) and 5 (25%) of the pregnant and non-pregnant women respectively had knowledge of rubella and how it could be transmitted. 15 (9.4%) of the pregnant women claimed to have been vaccinated against rubella while none of the non-pregnant women had ever received vaccination against rubella (Figure 1).
Risk Factors Because rubella is predominantly a childhood disease, situations that involve or result in having numerous children around were considered in this study as possible risk factors (Table 5). All the possible risk factors considered in this study were, however, not significantly associated with Rubella virus infection.
Analysis of the result showed that the difference observed in terms of age (pregnant women, χ2=8.891, df=5, p=0.113; non pregnant women, χ2=4.549, df=3, p=0.208) and the trimester of pregnancy (χ2=0.220, df=2, p=0.896) were not statistically significant. Similarly, the reproductive characteristics studied, socio-demographic data gathered and clinical characteristics observed were also not statistically significant for both pregnant and non-pregnant women (Tables 2 to 5). DISCUSSION Rubella IgM antibody was detected in 38.8% of the pregnant women and 40% of the non-pregnant women, indicating most probably that these women were infected recently. Nevertheless, the presence of anti-rubella IgM may also indicate reinfection or false positive results due to the presence of rheumatoid factors, cross-reacting IgM and infection with other viruses. Re-infection with rubella has been shown to be more frequent with vaccinated individuals than those infected naturally10 and this is less likely in this case. The use of sandwich ELISA with a specificity and sensitivity of 99.20% and 100% respectively for antibody detection in this study might also limit the possibility of false positive results. The prevalence in both groups is similar, indicating that both pregnant and non-pregnant women are similarly at risk of Rubella virus infection. This is a cause for alarm because the fetuses of the pregnant women infected might be predisposed to Congenital Rubella Syndrome. In addition, if any of the non-pregnant women become pregnant during the time of infection, the fetuses might also be at a higher risk because the risk of congenital infection is majorly limited to the first 16 weeks of pregnancy11. The prevalence is alarmingly higher than the report of previous studies such as 0.2% in the Western region of Turkey12, 1.1% in Ilorin13, 4.2% in Makurdi, Benue State14, 6.8% in Umudike, Abia State15 and 10% in Benin City16. The high prevalence observed between two different groups of women in different areas but within the same community suggests the occurrence of an outbreak during the time of the study. This is because outbreaks have been shown to occur and go unnoticed in developing countries like Nigeria17 and rubella-induced rashes when present are often misdiagnosed. The result goes further to confirm the increased incidence of rubella in Nigeria between 2010 and 2011 where a 8-fold increase from 450 to 3691 cases was reported18. This is alarming as infected infants can serve as an important means of viral circulation as virus from congenital infections persist after birth and those with congenital infections can infect others after birth for a year or more8. Pregnant women in their second trimester had the highest prevalence which contrast the results of the work carried out by Agbede et al13 and Ogbonnaya et al16 both of which had the highest prevalence in the first trimester. This may be due to the fact that majority of the pregnant women started seeking ante-natal care in their second trimester; as such the infection could not have been detected earlier. Although not statistically significant, older pregnant women had the highest prevalence for the study population. For the control population, however, the highest prevalence was seen in younger women. This contrast between the age group of infection may be as a result of increased exposure of these women to the predisposing factors to the virus. A study carried out in Abia16 supports this assertion. Seroprevalence of Rubella virus insignificantly increased with parity. This may be due to the fact that increase in parity predisposes to Rubella virus infection as a result of a longer interaction with more children and an infectious environment. We found little or no published work in Nigeria that reported the association between all the reproductive characteristics and risk factors considered in this study. However, Agbede et al13 reported that multigravidity was not a predisposing factor to rubella virus infection with primigravid women showing higher prevalence. Generally, the socio-demographic data of the pregnant women did not vary significantly with the presence of IgM antibody. Ogbonnaya et al16 was able to establish a higher prevalence in farmers in comparison to housewives, civil servants and traders. The highest prevalence in students may be attributed to the fact that Zaria is a town with many educational institutions. As such, many of the pregnant women are students in these educational institutions, which are mostly crowded thereby increasing their chances of being infected. The level of awareness and knowledge of rubella was low as previously reported by Mohammed et al19. None of the risk factors that were studied had any association with the risk of infection. However pregnant women in polygamous homes and those whose husbands were unemployed had the highest seroprevalence. Although, pregnant women who had rashes had a higher prevalence, none of the clinical symptoms presented by the women were associated with the risk of infection. Agbede et al13 in a similar study also found none of the clinical symptoms presented by the women in their study associated with Rubella virus infection. CONCLUSION The high seroprevalence of IgM antibody to rubella found amongst the pregnant and non-pregnant women who were asymptomatic indicates that rubella is endemic in Zaria and that minor epidemics are occurring and going unnoticed. Many pregnant and non-pregnant women in Zaria are susceptible to the virus and if they happen to come down with the infection during pregnancy, their fetuses might be predisposes to Congenital Rubella Syndrome. Rubella endemicity made the possible risk factors and clinical symptoms studied irrelevant. The level of awareness of Rubella virus and the infection it causes is very low and the antibodies were detected with higher frequency among pregnant women who knew about rubella. This indicates that awareness does not reduce the rate of infection, further emphasizes that vaccination remains the only means of prevention. REFERENCES
|
CrossRef Link